
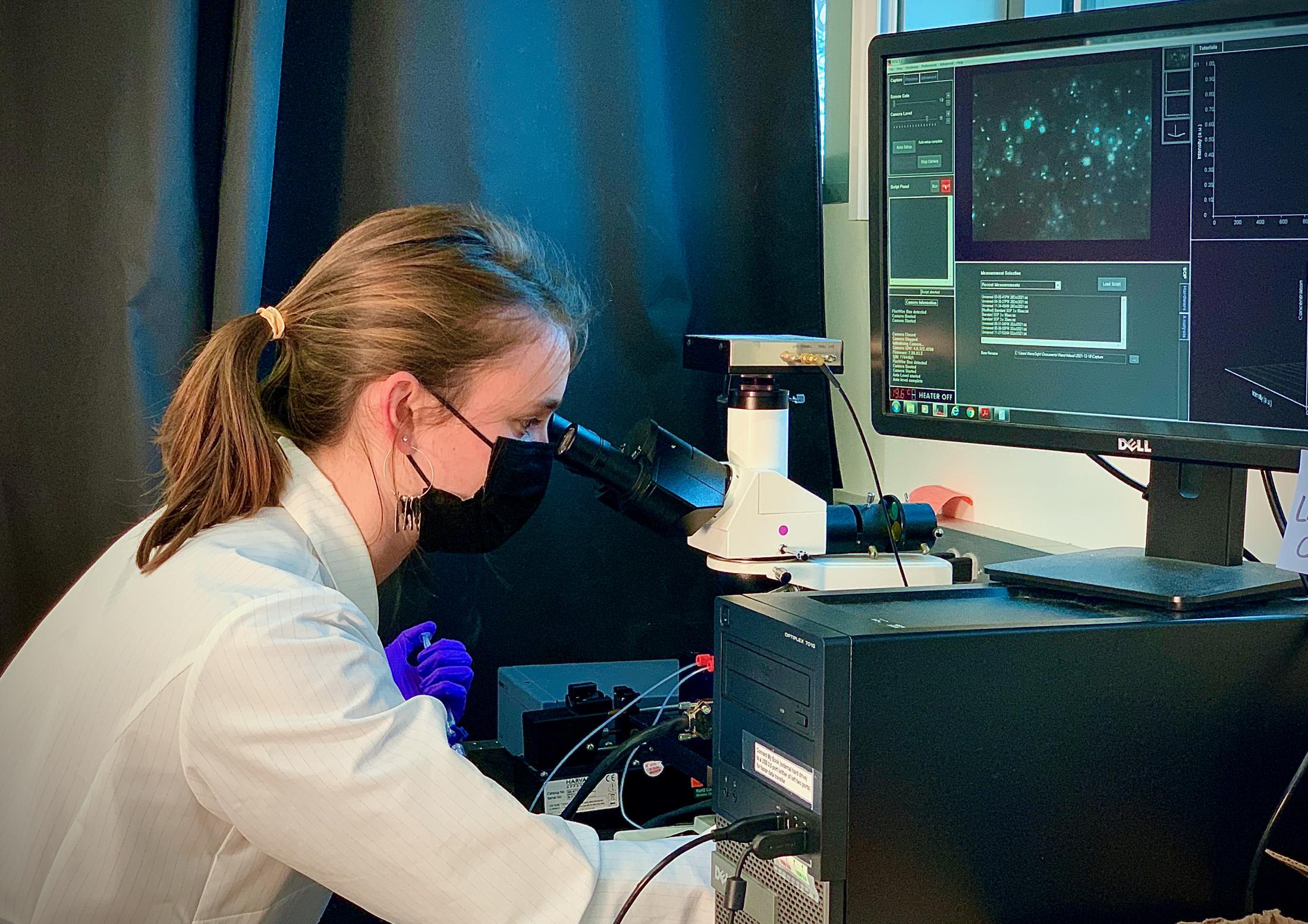
BME Graduate Student Rachel Mizenko Wins NIH Grant for Research Into Extracellular Vesicle Medicine Delivery for Multiple Sclerosis
Quick Summary
- These vesicles could allow drug delivery across the blood-brain barrier and prove useful for progressive multiple sclerosis
UC Davis' biomedical engineering (BME) student Rachel Mizenko just received an NIH National Institute of Neurological Disorders and Stroke (NINDS) F31 fellowship to develop an extracellular vesicular drug delivery system to help treat multiple sclerosis, under the mentorship of professor Randy Carney. Mizenko explains that this drug delivery system is important because it will allow medicine to reach the neural cells it needs to treat.
"Many drugs are given in excess in the hopes that enough will get to where it needs to go. This is what causes side effects, such as hair loss from chemotherapy - medicine acting on healthy tissue. When getting to the brain this issue is exacerbated because the brain has developed an extremely tightly controlled barrier between itself and blood vessels. Very few drugs can effectively get through this barrier, and this is thought to be one of the reasons that there has been such little progress in treating progressive MS."
Extracellular vesicles (EVs) are useful tools for drug delivery as some types of them can circumvent the blood-brain barrier. They are nanoparticle messengers produced by cells to transport information across the body. Proteins on their surface allow some EVs to penetrate the brain and others to target specific cell types. Mizenko is teasing out which EVs are the best kind to use for multiple sclerosis treatment.
Multiple sclerosis can be split into two main categories: relapsing-remitting and progressive forms. Relapsing-remitting disease comes in waves, where a person experiences symptoms, such as weakness and difficulty walking, and then recovers fully or partially. There are a number of drugs available that can decrease the frequency and severity of these relapses which are mostly aimed at calming the immune system.
In progressive multiple sclerosis, the loss of bodily functions is permanent and symptoms progressively worsen over time. Some therapies are FDA-approved for progressive multiple sclerosis, but they are ineffective for many patients.
As Mizenko points out, her work is targeted to help these patients. "One reason people believe progressive MS is so hard to treat is because the diseased cells are caught behind the blood brain barrier. Our drug delivery system is specifically tailored for these individuals with progressive forms of MS to get past this issue of the tight blood brain barrier to slow or stop this disease progression."
Right now the main goal for multiple sclerosis treatment is to slow progression of the disease. "Obviously, someday we'd love to have a treatment that can reverse the symptoms or cure the disease but there is just too much that we don't know about the disease right now. For example, how much of disease progression is from immune cell activity? Why do people switch from a relapsing-remitting form to progressive forms? Until we know these answers, we'll have to focus on slowing or stopping progression. However, determining how to truly stop progression especially for individuals with progressive forms of the disease is going to be a major stepping stone in understanding the disease. The more we understand how to control symptoms the better chance we have at curing MS completely."
Mizenko's lab's engineered vesicles will be composed of three parts: EVs that efficiently cross the blood-brain barrier, EVs that target oligodendrocyte progenitor cells (to which they are hoping to deliver the medicine), and a therapeutic micro-RNA. These need to be cell-produced rather than synthetic EVs because there are aspects to the messaging capabilities that scientists don't yet understand (i.e. cholesterol content, glycocalyx, lipid ratios).
They will begin by identifying which existing cell-produced EV population works best for its intended functions by testing EVs from different cell sources. Some can cross the blood-brain barrier and others can target oligodendrocyte progenitor cells, and they hope to find a population that can do both efficiently, or fuse together EVs isolated from different cells that can perform each function.
Mizenko explains her process in more detail. "For this reason, we will be fusing each optimized population to combine the proteins necessary to reach our drug delivery goal. Finally, the synthetic microRNA will be loaded into these fused EVs to make our final engineered vesicles. This allows a single vesicle to share the proteins necessary to carry the therapeutic micro-RNA from the bloodstream (where we'll inject it) all the way to the brain. While we optimize these functions, we'll be working to understand what properties or which proteins mediate these functions so that similar drug delivery systems can be used for other diseases.”
Carney is an exceedingly proud mentor, “This grant is the culmination of three years of dedicated work in the lab by Rachel, gathering data to focus her ideas even in the midst of the COVID pandemic, when it was very tough to even step foot in the lab. She is a bright young scientist and that fact that her brilliant idea to engineer EVs to combat MS is being recognized by the NIH is a testament to her talent and hard work. This is just the first big step in what I believe will be many accomplishments for Rachel, she is going to do big things!”
