FASEB Journal Spotlights UC Davis Researchers’ Work on Stem Cell-Based Neurological Therapies
‘A perfect example of researchers collaborating for real change’
UC Davis researchers working on in-utero stem cell-based therapies are excited to have their work highlighted in the latest edition of the FASEB Journal.
In the new article – “Neuroprotective Effect of Placenta-Derived Mesenchymal Stromal Cells [PMSCs] -Role of Exosomes" – researchers from the UC Davis Biomedical Engineering Department and UC Davis School of Medicine, as well as from Shriners Hospital for Children – Northern California, share possible strategies to use human placenta stem cells to provide protection to neuronal functions for infants diagnosed with spina bifida and similar congenital and neurological conditions.
“We’re thrilled to have our article included in the FASEB Journal because it’s an important study for our program, outlining some of the potential mechanisms of action of PMSCs,” said senior author of the study Dr. Aijun Wang of the UC Davis Biomedical Engineering Department and School of Medicine (Surgery Department). “It sets the foundation for potential applications of PMSCs for neurological diseases including spina bifida and many others.”
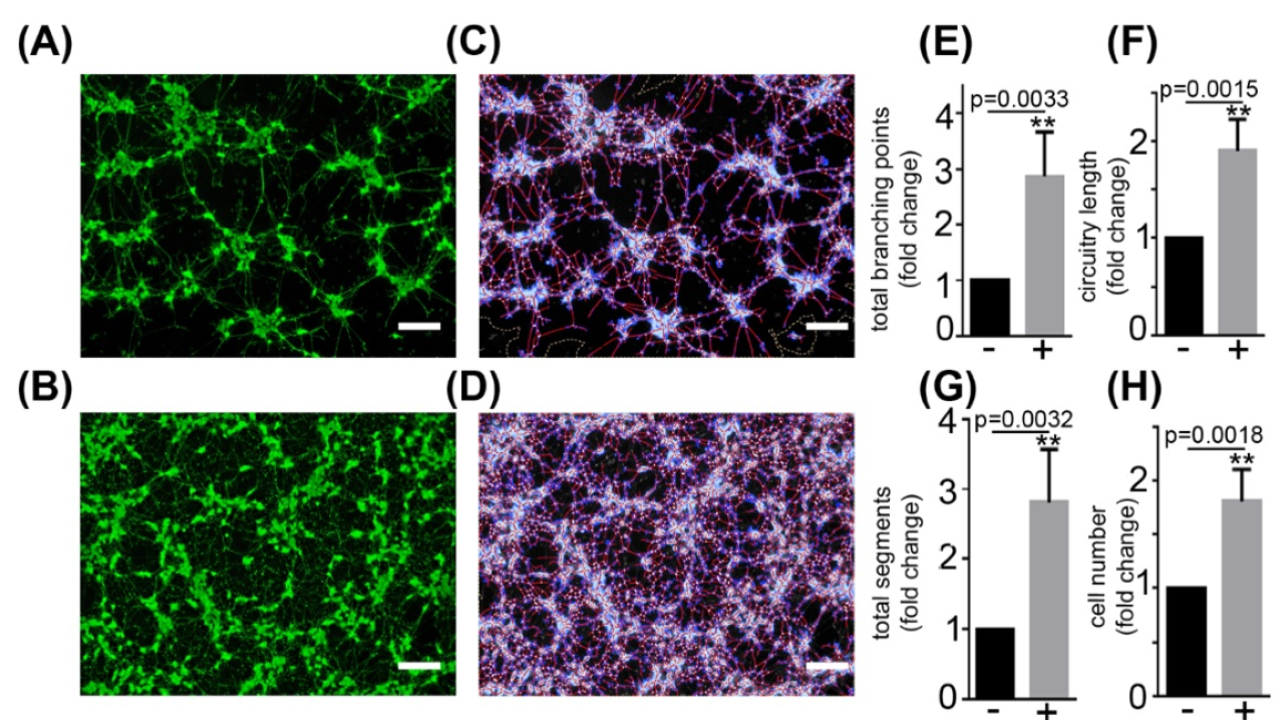
In the FASEB Journal article, the team members share how human PMSCs – and especially their exosomes (vesicles secreted by a cell consisting of liquid enclosed by a lipid bilayer) – contain materials with a high potential to protect fetuses’ neural materials during development. Using human PMSCs from four donors, they tested the exosomes’ neuroprotective effects and functions and identified proteins in the exosomes that could play a role in improving or strengthening embryonic neural development.
While the authors note their previous related cell-level therapies for lambs with surgically induced spina-bifida-like symptoms have shown positive results -- with greatly improved motor functions as compared to control animals – the data outlined in this new article help lay the groundwork and identify the potential mechanisms for the team’s ongoing efforts to translate these earlier cell-based therapies into possible solutions for human infants with neural congenital conditions.
“Working with Prof. Wang and the rest of the team to develop the use of exosomes – these tiny, therapeutic nanoparticles – to combat diseases affecting infants is a perfect example of researchers collaborating for real change,” said coauthor Dr. Randy Carney, also of the UC Davis Biomedical Engineering Department. “There are so many directions for us to explore together to make a difference for children – it’s very exciting!”
“We limited this study to the neuroprotective function of the placenta cells, but they very well could impart several other biological functions,” added Wang, noting team members already are looking forward to continuing their line of research. “Our findings also open up the possibility of therapeutic applications of the cells’ extracellular vesicles, implying the potential of a new stem cell-based, cell-free therapy for various diseases and conditions. The approach can be used not only for spinal-cord injuries, but also for other neurological disorders where neuronal death is associated.”
