
Pioneering New Technology to Study Heart Diseases at the Cellular and Molecular Level
Professor Ye Chen-Izu collaborates across the College of Engineering and School of Medicine to make discoveries about heart diseases
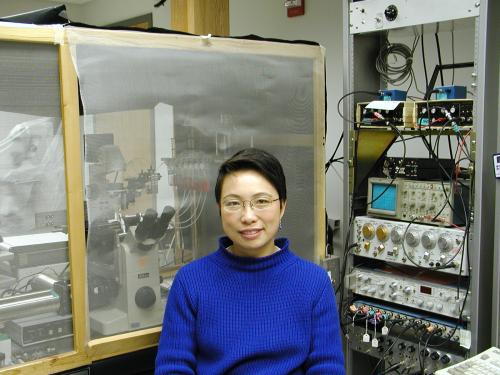
Dr. Ye Chen-Izu, director of the Cardiac Signaling Lab, leads an interdisciplinary team of researchers to study how the heart pumps blood to meet the body’s changing needs and why high blood pressure can cause heart diseases.
Succeeding in this research has necessitated pioneering a series of innovations, such as the lab’s most recent development of “cell-in-gel” technology.
With heart disease remaining the number one cause of death in the United States, Chen-Izu's lab's research into heart diseases is as relevant and urgent as ever. The lab’s mission is to translate breakthrough research findings to develop new drug therapies to prevent and treat heart diseases more effectively.
An engineering approach to studying the heart as a “smart” pump
As part of the College of Engineering and School of Medicine, Chen-Izu’s team has approached work with engineering expertise and an interdisciplinary mindset.
“According to control theory in engineering, we know that a dynamic system with closed-loop feedback enables a powerful property called autoregulation,” she said. “The heart can sense the change of the mechanical load and adjust its contraction to compensate for load changes. This is at the forefront of our research to combine our expertise in engineering and biology to study the heart as a smart pump with autoregulation.”
Solving long-standing mysteries through new technologies
The heart constantly operates under varying mechanical loads. For example, when someone is lying down to rest, the body’s demand for blood flow is different from when engaged in a stressful physical activity, like exercise or shoveling snow.
Yet, how the heart senses blood pressure and regulates its contractions to provide sufficient blood flow has been a long-standing mystery. A mystery that her team has recently helped to solve, thanks to creating new technologies along the way.
For decades, Chen-Izu has been studying three dynamic systems of the heart, beginning with the electrical system, then the calcium signaling system, and the mechanical contractile system. Her lab has made technological advances throughout each research stage, such as inventing the “action potential-clamp sequential dissection” method, which enabled the team to fingerprint the changes in many ion channels that contribute to heart diseases.
Interdisciplinary collaboration led to new technology – and discovery
Since starting her lab at UC Davis, Chen-Izu has developed interdisciplinary collaborations to invent new technologies. In partnership with Dr. Kit S. Lam, a chemist and cancer doctor at UC Davis, the team invented cell-in-gel technology to control 3-D mechanical stress on heart muscle cells.
“Now, we can embed a single muscle cell in the hydrogel and stimulate the muscle to contract against the resistance in this tissue-like environment. The gel is transparent, so we can look deep into the cell to study the molecular events under the microscope.”
Thanks to this “cell-in-gel” technology, they have made fascinating discoveries.
“We found that even a single muscle cell is able to sense the mechanical load and autoregulate its contraction to compensate for load changes. This means that the heart’s ability to autoregulate contraction starts at the single-cell level.”
Chen-Izu also collaborates with Professor Leighton T. Izu, a mathematician at UC Davis, and with Professor John Shaw, an aerospace engineer at the University of Michigan, to develop quantitative models to study the mechanical stress in heart cells. Such rigorous mechanical analyses are needed to understand why high blood pressure leads to heart diseases.
Translating research discoveries to new drug therapies is next
When a person has high blood pressure, the mechanical load is too high over a long time. This often leads to heart diseases, such as enlarged hearts, rhythm loss, and eventual heart failure. That’s why translating the lab’s discovery into drug treatments is so critical.
Chen-Izu said discovering how the heart muscle operates at the single-cell level will help in two areas of drug research and development. First is when new drugs are being developed to treat various diseases. Some may cause heart damage as a side effect. Therefore, the Food and Drug Administration (FDA) mandates that all new drug candidates undergo cardiotoxicity screening. Chen-Izu's lab’s research will be translated to industrial applications to improve that screening process. Her next project is to develop high-content and high-throughput cardiotoxicity screening technology. The second area is being able to screen millions of drug candidates to discover new drugs for treating heart diseases.
“I want to mention the importance of being optimistic,” she said. “Especially as a scientist and bioengineer – I’m optimistic that we humans still have the power to improve our situation.”
