NIH funds project to model atrial fibrillation with heart-on-a-chip
Atrial fibrillation (AF) is an irregular heartbeat caused when the heart’s upper chambers beat chaotically and out of sync with the lower chambers, leading to a variety of health problems including stroke and death. Nearly 1 in 10 people over the age of 65 suffer from AF, with around $6 billion spent every year on healthcare, making its treatment a priority for the healthcare industry.
Conventional medications for AF restore normal heart rhythm but can have unpleasant side effects. More recent invasive treatment options such as ablation are also effective but not curative as they do not target the cellular abnormalities that characterize AF.
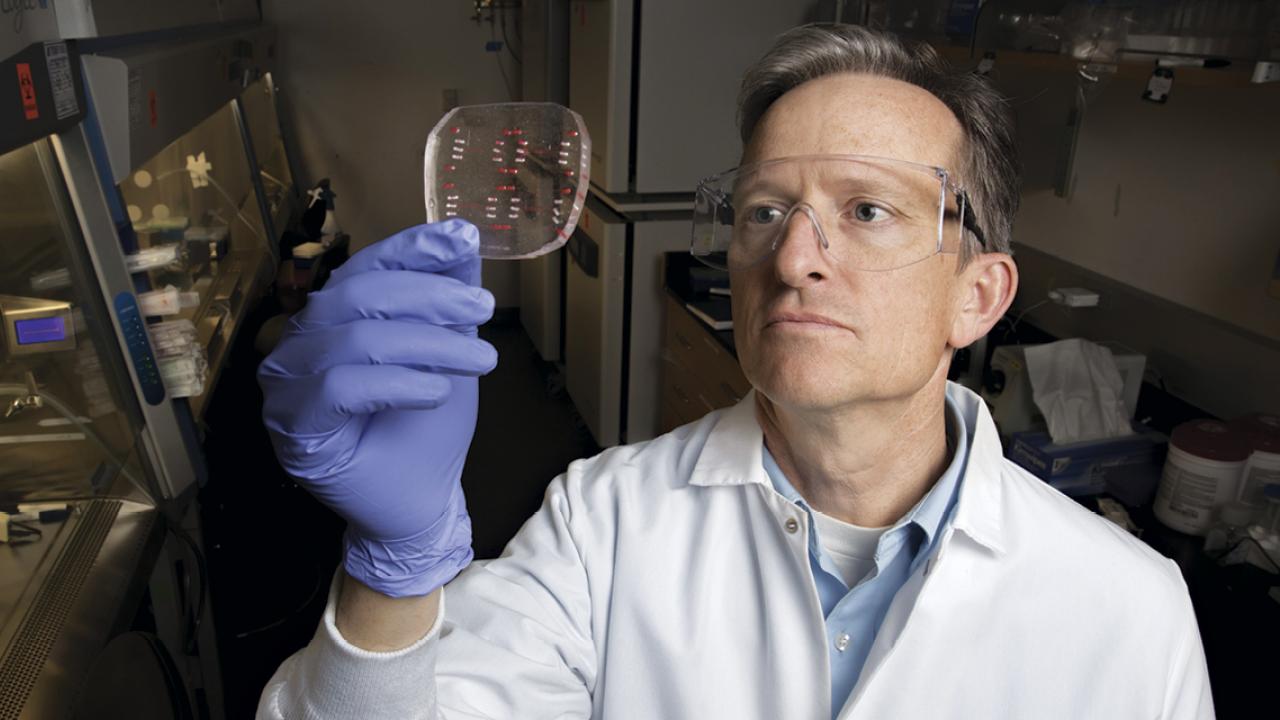
But that might change with a bold new project, led by UC Davis Biomedical Engineering professor Steven George, to create AF-like conditions using live human heart cells in a functioning model of a human heart on a tiny chip. With $6 million in funding from the NIH, over the next 5 years George and his collaborators at Washington University in St. Louis plan to create atrial tissue from a patient’s own stem cells, and induce changes in the cells using CRISPR technology (“gene editing”) to alter their protein expression so that they conduct electricity in a pattern resembling that seen in AF. Then, the project aims to reverse this pattern with a gene editing strategy delivered by a modified virus that only targets the atria.
“Heart muscle cells ‘connect’ to each other to allow electrical current to pass between them, and these connections are altered in patients with AF. We can’t reproduce true AF on our chip, but we can reproduce the features of how cells communicate electrically that predispose a person to AF, and that’s what we’re trying to do in this new project,” George explained.
White blood cells or skin cells obtained from a person will be converted into induced pluripotent stem cells, which are capable of forming into any type of tissue. George’s lab will then treat these stem cells to conditions that encourage them to form the heart muscle cells found in the atria. The cells that make up the ventricle and the atria are so similar that growing only atrial heart muscle cells is a delicate task, but George’s lab has already done some initial work in this area, and he believes they will succeed.
Rather than target proteins in the cell membrane like conventional treatments, George’s approach will target proteins “upstream” that orchestrate the production of the downstream membrane proteins (ion channels).
“What’s new is not directly targeting the ion channels, but rather the upstream proteins that influence them, and only in the atria,” he said.
If successful, the treatment will be reversible and not permanently change the “genetic code” of the patient.
The project is part of a 5-year NIH program dubbed “Tissue Chips 2.0”, which funds research to create and intervene in models of disease on laboratory chips. Co-Principal Investigators on the project are Stacy Rentschler, MD, PhD, and David Curiel, MD, PhD, both of whom are at Washington University St. Louis. The tissue engineering and lab-on-a-chip work will be done at UC Davis, while the gene therapy and ex vivo testing will be done at Washington University in St. Louis.
